Parodontitisbehandlung – Vorbeugen und Pflegen:
Parodontitis (im „Volksmund“ Parodontose genannt) ist die Erkrankung des Zahnbettes. Etwa 80% aller Menschen leiden unter dieser Krankheit. Die Parodontitis verläuft meistens schmerzlos und zieht sich über Jahre hin. Die Erkrankung ist in der Hauptsache die Folge von nicht optimaler Mundhygiene. Eine einseitige und vitaminarme Ernährung kann aber, ebenso wie übermäßiger Nikotingenuss, die Ausbildung der Erkrankungen fördern.
Eine beginnende Parodontitis lässt sich an bestimmten Symptomen, wie zur Blutung neigendes Zahnfleisch und unangenehmer Beigeschmack, erkennen. Durch regelmäßige Zahnreinigung und Behandlung des Zahnfleisches, vielseitiger, gesunder Ernährung, sowie einer mindestens halbjährlichen Untersuchung beim Zahnarzt kann einer Parodontitis wirksam vorgebeugt werden.
Krankheitsverlauf
Bei der Parodontitis kommt es zuerst immer zu einer Entzündung des, den Zahnhals umgebenden, Zahnfleischsaumes (Gingivamanschette). Anschließend wandert die Erkrankung weiter und dringt in die Tiefe des Zahnbettes ein, in das die Zähne eingelagert sind (Alveolen). Das Zurückziehen des Zahnfleisches lässt sich nicht mehr aufhalten und die Knochenfächer werden immer kleiner. Die Zähne werden locker und stören beim Sprechen und Kauen. In den meisten Fällen lässt sich eine Entfernung der Zähne zu diesem Zeitpunkt nicht mehr vermeiden.
 |
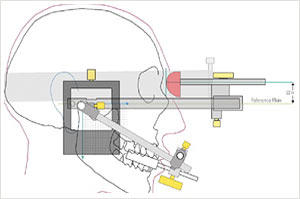
Ultraschallsystem PerioScan
Foto mit freundlicher Genehmigung von Sirona Dental Systems GmbH |
Parodontitisentwicklung – Früherkennung
Eine Parodontitis kann an folgenden Merkmalen erkannt werden: die Zähne werden länger, weil sich das Zahnfleisch zurückzieht, es entsteht Mundgeruch, die Frontzähne wandern und kippen nach außen, es entstehen Zahnlücken, die vorher nicht waren. Frühzeitige Erkennungsmerkmale sind verstärkte Blutungsneigung des Zahnfleisches und ein unangenehmer „Beigeschmack“.
Parodontitisentwicklung – Selbsthilfe
Vermieden werden kann eine Parodontitis durch regelmäßige Zahnreinigung und Behandlung des Zahnfleisches. Eine ausgewogene, gesunde Ernährung spielt ebenfalls eine sehr große Rolle, sowie die halbjährliche Untersuchung beim Zahnarzt. Wenn das Zahnfleisch eine blass-rosa Farbe hat, ist es gesund. Feine zipfelförmige Ausläufe, Papillen genannt, füllen die Zahnzwischenräume aus.
Entzündetes Zahnfleisch bekommt eine starke Rotfärbung und neigt zum Bluten. Beim Zähneputzen kann das sehr schmerzhaft sein.
Vorsorge Zähneputzen – aber richtig!
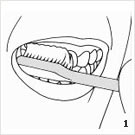
Im Folgenden wird eine, von vielen angewandte Zahnputztechnik vorgestellt.
Entsprechend dem jeweiligen Alter (Kind oder Erwachsener), mögliche Vorerkrankungen berücksichtigend, je nach dem, ob elektrisch oder mit einer Handzahnbürste geputzt wird, gibt es individuelle Unterschiede in der optimalen Putztechnik. Die für Sie richtige Putztechnik erläutern wir Ihnen gern in einer Prophylaxesitzung in unserer Praxis.
Nach jedem Essen (3 x täglich) sollten die Zähne geputzt werden, so können keine schädlichen Zahnbeläge entstehen.
Die empfohlene Zeit für die Zahnreinigung beträgt 3 Minuten.
Der Mund wird zuerst kräftig ausgespült und das Wasser durch die Zahnzwischenräume gepresst, um bereits die frischen Speisereste zu lösen.
Anschließend werden zuerst die Außenflächen der Zähne mit Zahnpasta und Zahnbürste gereinigt. Bei leicht geöffnetem Mund wird am letzten Backenzahn im linken Oberkiefer begonnen. Es werden, mit leichtem Druck, kleine kreisende Bewegungen an jeweils 2 – 3 Zähnen durchgeführt, – das Ganze ca. 10 Mal. Anschließend wird die Zahnbürste etwas weiter vorn wieder angesetzt. Auf diese Weise werden die Zähne in kleinen Abschnitten, bis hin zur rechten Seite des Oberkiefers gesäubert. Gleiches Vorgehen versteht sich im Unterkiefer. Es wird unten links am letzten Backenzahn begonnen, die Innenflächen sollten nicht vergessen werden. Zum Schluss werden noch alle Kauflächen geputzt. Jetzt ist Hin- und Her-Schrubben erlaubt. Anschließend wird der Mund wieder kräftig ausgespült, damit alle weggeputzten Speisereste entfernt werden. Aufgepasst, beim Zähneputzen von den Seiten nicht zu starken Druck ausüben, sonst ziehen sich die filigranen Gewebe um die Zähne zurück und man „schrubbt“ sich die Zahnhälse frei. Mit einem maximalen Druck, der etwa 200 Gramm entspricht, soll geputzt werden. Nicht die Kraft, sondern die Zeit ist entscheidend.
- Reinigung mit Zahnbürste
- Reinigung mit Zahnseide
- Bewegungsablauf innen
- Bewegungsablauf außen
Es gibt noch viele andere Dinge, die berücksichtigt werden sollten. Wir als Praxisteam können hier noch viele Tipps in der Prophylaxe geben.
Was ist zu tun, wenn sich die ersten Anzeichen einer Parodontitis zeigen?
Der erste Weg führt in die Zahnarztpraxis. Hier kann festgestellt werden, ob es sich um eine Parodontitis handelt, welchen Schweregrad sie hat und welche Therapieschritte notwendig sind.
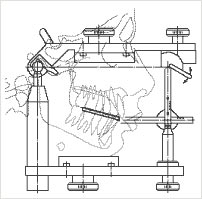
In der Regel wird sich eine professionelle Zahnreinigung anschließen. Nach einigen Vorbehandlungsterminen wird dann der Bereich tief in der Tasche gereinigt. Hier kommen in der Regel spezielle Handinstrumente zum Einsatz. Zur Unterstützung bzw. zur Optimierung des Behandlungsergebnisses werden in unserer Praxis zusätzlich auf Wunsch zum Beispiel Ultraschallgeräte, die speziell festgelegte Bewegungen ausführen, eingesetzt.
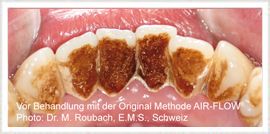
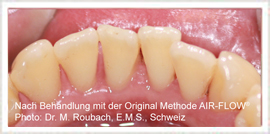
Fotos: mit freundlicher Genehmigung der Firma Dürr Dental
- Der Vector™
- Bild 2 – 4: Der Vector™ im Einsatz
Neben dem Soniflex, das elliptische Bewegungen vollführt, wird das Vektorsystem verwendet. Bei diesem wird ein Pulver-Flüssigkeitsgemisch in Ultraschallschwingungen versetzt, wodurch man die Zahnwurzel sanft von Ablagerungen befreit und dabei gleichzeitig die Wurzel poliert.
Als weitere, unterstützende Maßnahme kann der Laser zum Einsatz kommen. Dieser ist in der Lage, ohne zusätzliche Medikamente Bakterien in den Zahnfleischtaschen zu beseitigen bzw. abzutöten. Weiterhin kann er erkranktes Gewebe entfernen und die Voraussetzung schaffen, dass das Zahnfleisch wieder am Zahn anwächst (Deepithelisierung).







































 Mit den ersten Zähnen wird es auch Zeit für die erste Kontaktaufnahme mit dem Zahnarzt. Dieses erste Kennenlernen sollte nicht erst geschehen, wenn Schokolade & Co die ersten Spuren auf den Zähnen hinterlassen, sondern die Gelegenheit, das Vertrauen des Kindes zu gewinnen besteht schon viel eher. Zum Beispiel wenn ein Elternteil zu einer Kontrolluntersuchung die Praxis besucht.
Mit den ersten Zähnen wird es auch Zeit für die erste Kontaktaufnahme mit dem Zahnarzt. Dieses erste Kennenlernen sollte nicht erst geschehen, wenn Schokolade & Co die ersten Spuren auf den Zähnen hinterlassen, sondern die Gelegenheit, das Vertrauen des Kindes zu gewinnen besteht schon viel eher. Zum Beispiel wenn ein Elternteil zu einer Kontrolluntersuchung die Praxis besucht. bleiben Zähne lange gesund und stark und die ersten Besuche können einem „ Probesitzen auf dem fahrbaren Zahnarztstuhl“ entsprechen.
bleiben Zähne lange gesund und stark und die ersten Besuche können einem „ Probesitzen auf dem fahrbaren Zahnarztstuhl“ entsprechen.